The Gut-Brain Axis: How The Vagus Nerve Impacts Digestion
Some of the links in this post might be affiliate links. This means that if you click on the link and make a purchase, I’ll receive a small commission – at no extra cost for you, which helps me cover the costs for this blog.
Gut health has become one of the most widely discussed topics in the health and wellness world — and for good reason. Today, it seems like nearly everyone is struggling with digestive issues: whether it’s IBS, gastritis, Crohn’s disease, colitis, GERD, or a mysterious feeling of bloating, pain, and discomfort that doesn’t seem to fit neatly into a single diagnosis.
If you’re one of the lucky ones and don’t have gut issues, you probably know someone who does; In fact, nearly two-thirds of Americans experience symptoms like bloating, abdominal pain, diarrhea, or constipation on a weekly basis, according to recent data. The American Gastroenterological Association reports that over 60–70 million Americans actually have a digestive disorder (that’s a whopping 40% of the country), while the GI Alliance calls gut disorders "one of the Nation's most serious health problems" in terms of lost productivity, health care costs, and personal suffering.
I’m one of those people. This website was born from my own journey with chronic gut issues, which no medication or diet alone could seem to fix. After trial, error, unhelpful doctors, and plenty of frustration, I realized that the missing piece wasn’t just diet or supplements — it was my nervous system.
If you’ve been struggling with unexplained digestive symptoms and haven’t found answers through traditional routes, it might be time to take a closer look at your gut-brain connection.
Why? keep reading.
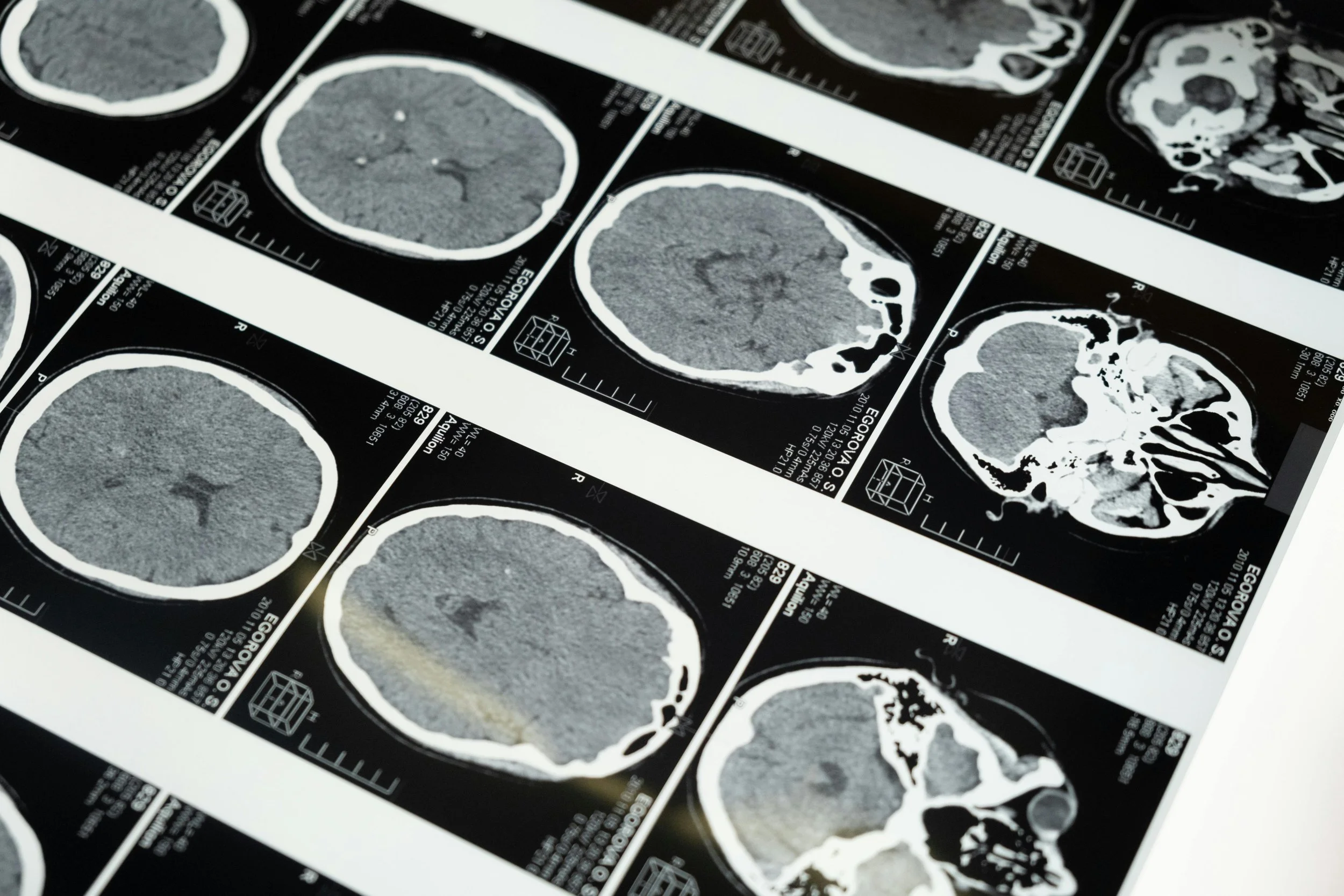
The Gut-Brain Axis: How The Nervous System and Digestive Health Intertwine
what is The Autonomic Nervous System?
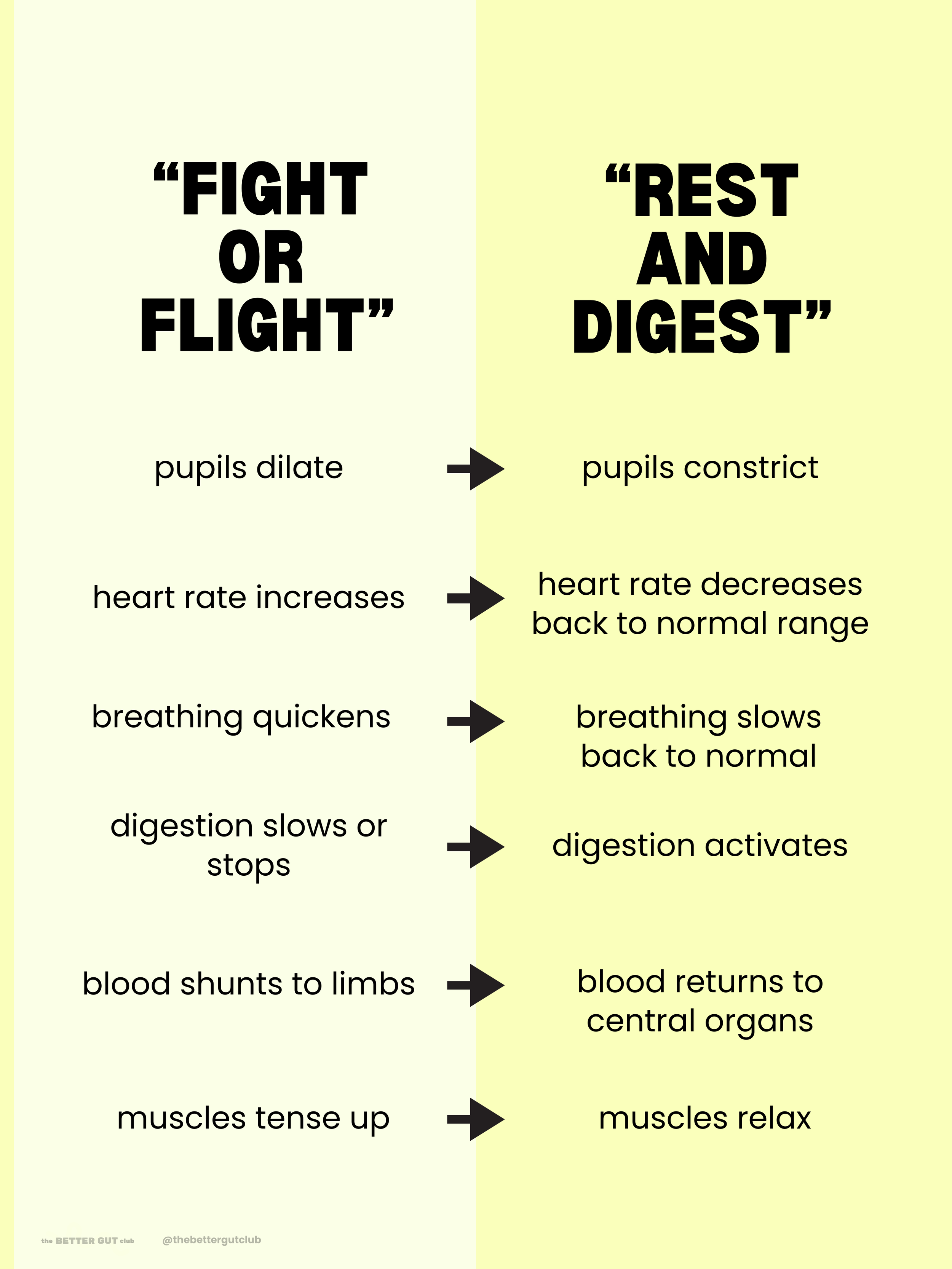
Your autonomic nervous system (ANS) controls the body functions you don’t consciously think about: breathing, heartbeat, blood pressure, and of course digestion. It’s made up of two key branches, of which either one or the other is always activated:
The sympathetic nervous system, which activates your "fight-or-flight" response when you’re stressed
The parasympathetic nervous system, which brings you back to a relaxed state so you can “rest and digest”
When we go into “fight-or-flight” mode, what’s happening is the sympathetic branch of the ANS is being activated. Our pupils dilate, our senses become heightened, and our heart rate increases; this is because, evolutionarily, our body is preparing to fend off any dangers that are coming our way. How so? The blood coursing through our body is shunted away from our digestive organs and into our arms and legs so that energy is utilized to run and fight; as a result, digestion is put on the back-burner whenever fight-or-flight is activated.
Thankfully, we also have the parasympathetic nervous system, which calms us down. It slows the heart rate and redirects blood flow back to the digestive organs. It’s the system responsible for restoring balance to the body, which is why it's known as the "rest and digest" mode. Ideally, we spend most of our lives in this state unless there is a danger present.
These two branches shift in dominance as we go about our day, interpreting stimuli and reacting emotionally. This seesawing has a profound effect on the way our gut functions.
Need help getting to the root of your gut issues?
Download my FREE Gut Health Symptom Assessment to uncover patterns in your digestion, energy, and mood
The Enteric Nervous System: The "Second Brain" in Our Gut
The vagus nerve is the main line of communication between the brain and the gut. It’s the longest cranial nerve in the body and is part of the parasympathetic system. When activated, it stimulates digestion, secretion, motility, and immune response in the GI tract.
Even more fascinating? Your gut has its own self-contained network of neurons known as the enteric nervous system (ENS). Often called the "second brain," the ENS regulates digestion independently of the brain. It produces the same neurotransmitters as the brain — including serotonin, dopamine, and norepinephrine — which is why changes in gut function can affect mood, cognition, and energy levels.
Dysregulation of the ENS has been linked to:
Mood disorders like anxiety and depression
Cognitive issues including brain fog and difficulty concentrating
Immune dysfunction, triggering food sensitivities and inflammation
Sleep disturbances due to impaired serotonin and melatonin production
Malabsorption of nutrients, which leads to further system-wide depletion
Disrupted gut motility, causing constipation, diarrhea, or gastroparesis
Chronic stress and trauma can majorly affect these systems, leading to cycles of gut dysfunction and emotional imbalance.
Ready to take charge of your own health?
Get my FREE Gut + Mood Tracker Toolkit to track your symptoms and start uncovering patterns!
Can We Fix It?
While these systems may seem automatic and out of our control, and it takes time and consistency, but we can influence the nervous system and gut-brain axis through intentional daily practices. If the source of your digestive issues is indeed a dysregulated nervous system, supporting your vagus nerve is one of the most effective ways to shift into parasympathetic mode and get your digestion back on track. Of course, if other variables are involved, like parasites, gut flora imbalances, or genetic disorders, healing may be a little more complicated (but not impossible!)
How to manually stimulate the vagus nerve
Breathwork
Deep belly breathing stimulates the vagus nerve and helps shift the body out of fight-or-flight. When you breathe diaphragmatically, you mechanically activate vagal pathways that signal safety to the brain. This slows heart rate, reduces muscle tension, and increases heart rate variability (HRV), a key marker of strong vagal tone.
Even 3–5 minutes of box breathing (4 counts in, 4 counts hold, 4 counts release, 4 counts hold, repeat) can create measurable shifts in your nervous system.
Yoga
Gentle movement, twisting postures, and breath-focused flows in yoga support vagal tone and help regulate stress hormones. Twists and forward folds gently compress and release the abdominal organs, sending sensory feedback to the vagus nerve that encourages relaxation and digestive motility.
Yoga also strengthens the mind-body connection by pairing movement with breath, one of the vagus nerve’s favorite ways to activate. Practicing a few times a week is enough to build long-term resilience and improve emotional regulation.
Meditation
Meditation reduces sympathetic activity and enhances parasympathetic tone, allowing the vagus nerve to take the lead. Regular practice increases gray matter in brain regions responsible for emotion regulation and stress inhibition, which reinforces a calmer baseline state.
Over time, meditation improves your ability to recover from stress more quickly (both emotionally and physically) and supports smoother digestion by signaling the gut that it’s safe to function normally. Remember to have patience with yourself and that meditation doesn’t have to be perfect (and rarely is - we’re only human!).
4. Singing/Humming
Singing or humming stimulates the vagus nerve through vibration of the vocal cords and activation of the muscles in the back of the throat. These vibrations directly engage vagal pathways connected to breathing and heart rate regulation, making these simple actions surprisingly powerful tools for nervous system support. This is also why singing can feel emotionally releasing or grounding…it's a natural parasympathetic booster that improves mood almost instantly!
5. Herbal Support
Adaptogens like ashwagandha, reishi, and holy basil help the body modulate stress responses by balancing cortisol and supporting adrenal resilience, which indirectly enhances vagal tone.
Nervines — such as chamomile, skullcap, lavender, and lemon balm — work more directly on the parasympathetic system to calm the mind, relax the digestive tract, and soften muscle tension.
These herbs don’t “force” relaxation, rather they help create the internal conditions where the vagus nerve can activate naturally. Keeping a few of these herbs in your tea cabinet makes it easier to support a calm and grounded baseline.
want more ways to regulate?
Discover the most widely-loved products of 2025 that have helped people heal their nervous system naturally
final thoughts
The gut-brain connection is no longer a gray idea — it’s vital to understanding chronic digestive issues, emotional regulation, and whole-body health. If nothing else has worked, supporting your nervous system may be the missing piece.
It certainly was for me!
If you’ve been living in a cycle of symptoms, supplements, and still feeling stuck, I hope this article gave you some clarity and new tools to explore. Healing is never linear, but you have more power than you think.
Ready to begin your gut healing journey?
The FREE 3-Day Gut Reset Kit includes a gentle meal plan, grocery list, and healing rituals to help you reset — no overwhelm required.
Or, if you’re ready for a longer reset, grab my 14-Day Gut Reset Recipe Book with 56 gut-healing meals, grocery lists, and simple support for real relief.
MORE ON THE BLOG
⬇
I am not a medical professional, nor do I claim to be. The information provided is not intended to be a substitute for medical treatment, but for educational purposes only. Please consult your medical care provider before using herbal medicine, particularly if you have a known medical condition or if you are pregnant or nursing.